Abstract
Objectives
The monitoring of fracture healing is a complex process. Typically, successive radiographs are performed and an emerging calcification of the fracture area is evaluated. The aim of this study was to investigate whether different bone healing patterns can be distinguished using a telemetric instrumented femoral internal plate fixator.
Materials and Methods
An electronic telemetric system was developed to assess bone healing mechanically. The system consists of a telemetry module which is applied to an internal locking plate fixator, an external reader device, a sensor for measuring externally applied load and a laptop computer with processing software. By correlation between externally applied load and load measured in the implant, the elasticity of the osteosynthesis is calculated. The elasticity decreases with ongoing consolidation of a fracture or nonunion and is an appropriate parameter for the course of bone healing. At our centre, clinical application has been performed in 56 patients suffering nonunion or fracture of the femur.
Results
A total of 39 cases of clinical application were reviewed for this study. In total, four different types of healing curves were observed: fast healing; slow healing; plateau followed by healing; and non-healing.
Conclusion
The electronically instrumented internal fixator proved to be valuable for the assessment of bone healing in difficult healing situations. Cost-effective manufacturing is possible because the used electronic components are derived from large-scale production. The incorporation of microelectronics into orthopaedic implants will be an important innovation in future clinical care.
Cite this article: B. Kienast, B. Kowald, K. Seide, M. Aljudaibi, M. Faschingbauer, C. Juergens, J. Gille. An electronically instrumented internal fixator for the assessment of bone healing. Bone Joint Res 2016;5:191–197. DOI: 10.1302/2046-3758.55.2000611.
Article focus
-
Can an electronically instrumented internal plate fixator help to determine bony consolidation and follow up the healing process in nonunions?
-
Is there any difference in radiological and mechanically assumed stability, which might decrease the need of radiological follow-up in the future?
Key messages
-
Wireless in vivo determination of elasticity is possible to determine bony healing of fractures and nonunions.
-
The system for electronic instrumentation of a locking plate internal fixator was found to be cost effective and can be realised with electronic parts from mass production.
-
Four different healing patterns were found.
Strengths and limitations
-
Additional revision surgery and bone grafts can be avoided without the need of extensive radiological follow-up examinations.
-
Significant suggestions when to increase weight-bearing depending only on the telemetric findings need a larger patient group to be evaluated in the future.
-
Muscular tension is effecting the measurements and needs to be considered for each patient.
Introduction
The assessment of bone healing in fractures or nonunions by radiograph appears trivial at first glance. However, it has been shown that it is a rather complex problem.1 There is no uniform definition of radiological criteria for a fracture to be considered healed. In the current literature, predominantly the criteria of bridging of the fracture with trabecular bone and bridging of the fracture in three cortices are used.2,3 In nonunions, due to the irregular shape of the gap, it is often nearly impossible to quantify the healing based on projection radiographs. In these cases, CT examinations are usually carried out.4
Moreover, studies have shown that it is problematic to correlate radiographic findings with mechanical stability. Clinicians were unable to determine the strength of a healing fracture on a set of radiographic images, or order radiographs according to stability.5-8
A measurement method of mechanical parameters appears to be a solution for the objective assessment of bone healing. In recent years, modern microelectronics have been increasingly applied in objects and devices of ‘ordinary life’. Electronic components have become cheap and provide powerful functions, despite their very small size.
In an interdisciplinary research collaboration between electronic engineers and clinicians, a low-cost miniature telemetric system was developed and incorporated into a femoral internal fixator to be applied specifically for the treatment of nonunions. The development of this innovation was funded by the German Mandatory Accident Insurance (DGUV) and by the German Federal Ministry of Education and Research (BMBF).
Preliminary results, including biocompatibility tests and initial clinical experiences, have been reported.9,10 The aim of this study was to identify different healing patterns using a telemetric instrumented femoral internal plate fixator in a series of applied clinical cases.
Materials and Methods
The telemetric system consists of a telemetry module which is applied to an internal multidirectional locking plate fixator, an external reader device with the appropriate antenna, a sensor for measuring externally applied load, and a laptop computer with processing software. The telemetry module comprises a strain gauge bridge and a 10 mm ×12 mm electronic circuit board with a microprocessor for processing and communication. The system allows for measurement of temperature via the temperature sensor in the microprocessor. Strain gauges are arranged on the rear side of the plate to measure bending of the plate. The telemetry module is coated with epoxy resin and bonded to the plate. The plate is a femoral internal fixator (litos/ GmbH, Ahrensburg, Germany) 200 mm long, 20 mm wide and 6.5 mm thick, with a waveform bridging the fracture site. In some individual cases, the telemetry electronics were also applied to custom-made implants. The system does not include a battery. The energy supply is realised electromagnetically via the reader device. This consists of an antenna of 10 cm in diameter placed on the skin and a mini portable electronic unit (8 cm × 5 cm × 2 cm). Additionally, the reader comprises a storage option with a SD card and an acceleration and motion sensor that can activate the device when the patient moves. The transmission of the data to the evaluation laptop computer is performed either via Bluetooth or via a USB cable. The force sensor for the measurement of an applied external force, e.g. under the foot, is also connected to the evaluation computer. The computer allows the storage of the data as well as the direct evaluation of a correlation between a telemetrically measured implant load and the externally applied load, in order to determine the elasticity of the healing bone.
The instrumented internal femoral fixator was applied in a consecutive series of patients with femoral nonunions referred to the BG Trauma Hospital Hamburg as well as one case each of an osteotomy, a segmental transport and a revision osteosynthesis during primary fracture treatment.
Intra-operatively, before internal fixation, all necrotic bone and soft tissue was removed from the nonunion/fracture gap. Cancellous bone grafting was performed in all cases. Post-operatively, patients were mobilised with partial weight-bearing starting with 10 kg. Weight-bearing was increased progressively according to clinical and radiological findings, with the telemetric results of the new technique considered as additional information.
Telemetric measurements were performed at an outpatient examination every two or four weeks, depending on individual patient follow-up logistics. A measurement consisted of three cycles of increasing and decreasing external loads with a sample rate of five per second and a whole duration of approximately 30 seconds (Fig. 1).
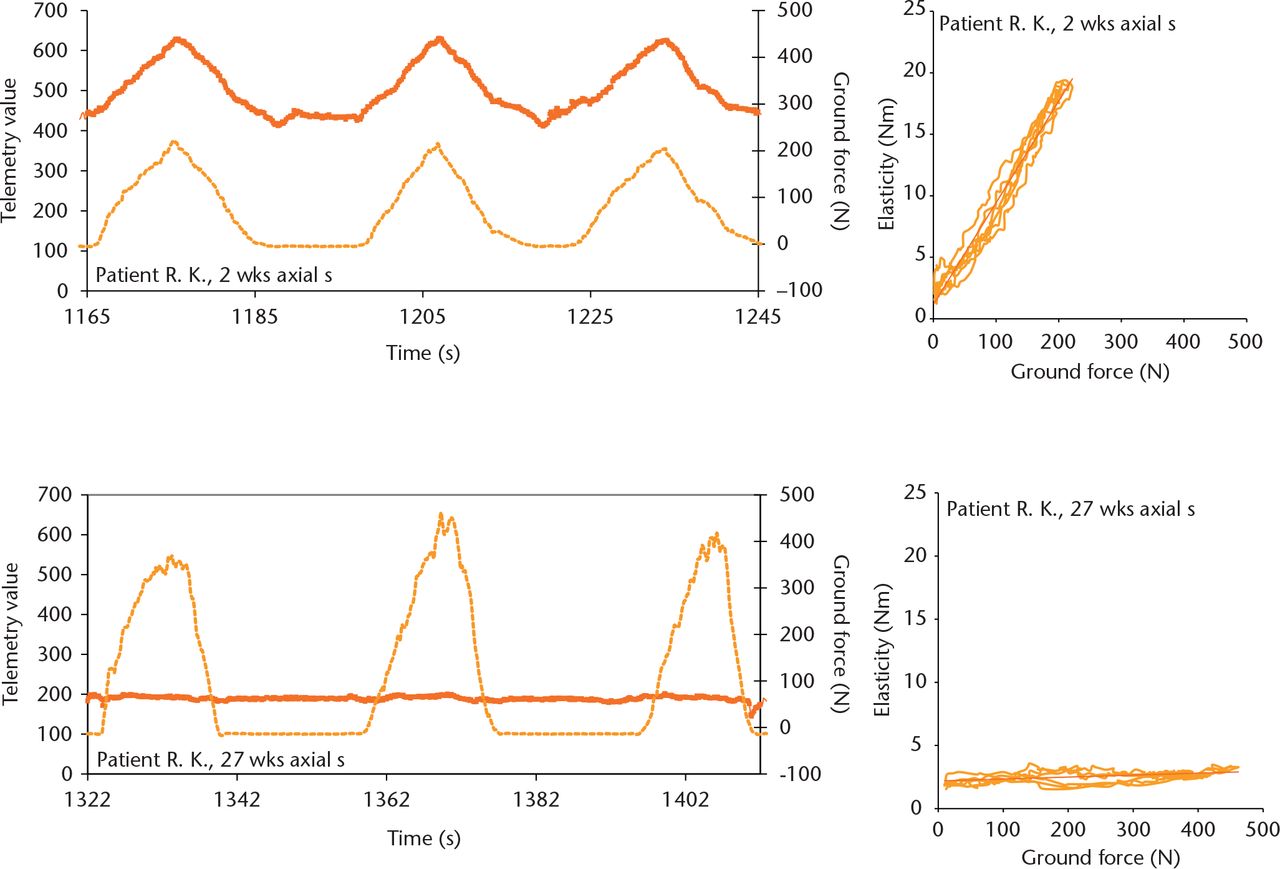
Fig. 1
Original recordings of externally applied load (dotted line) and telemetrically measurement implant load (solid line). Two weeks post-operatively (upper left), high implant loads were measured; the implant load was nearly gone by 27 weeks (lower left). Each measurement consisted of three cycles of increasing and decreasing external load. The corresponding slope of the regression line between externally applied load and measured fixator loads (upper and lower right) was calculated as the parameter of bone healing.
The slope of the regression line between externally applied load and measured fixator loads was calculated as the parameter for the elasticity of the osteosynthesis. A high slope, i.e. a significant increase of the implant load on application of the external load, indicates an unhealed bone; a low slope, i.e. a small increase in the plate load with external application of the load indicates a healing or healed fracture, as the healed bone is taking over most of the load (Fig. 1). To allow for inter-individual comparison of typically very different fracture shapes and fracture gap widths, the individual relative stiffness over time was calculated. The elasticity values of the different time points were divided by the maximum value obtained during the early healing process. The maximum value of stiffness was set at 100%. Clinical union was defined as full weight-bearing in the absence of pain or tenderness.3
Results
At the time of evaluation, the implant had been used in 56 cases. Treatment with the evaluated device was declared finished when clinical healing and radiological consolidation were achieved. In all cases, telemetric measurements of elasticity of the osteosynthesis had dropped below 10% of the maximum value in the early healing phase. A total of 47 patients met the criteria for completed treatment. The study includes 39 patients: 36 femoral nonunions after fracture, one nonunion after an Ilizarov segmental transport, one osteotomy and one revision osteosynthesis for primary fracture treatment. In the other eight patients, measurements were not possible over the entire healing period because of technical problems during the early development phase of the system.10
The age of the patients averaged 36 years (standard deviation (sd) 13); 34 patients were male, five female. Of the 39 patients 18 were smokers and 21 non-smokers. The type of nonunion was diagnosed as atrophic in 18 patients, oligotrophic in eight patients and hypertrophic in 11 patients. Intra-operative specimens confirmed bacterial contamination in 12 of 39 patients. The nonunion or fracture was localised to the middle third of the femoral shaft in 20 patients, in the proximal femoral shaft in eight patients, the distal femoral shaft in eight patients, the proximal joint region in two patients and the distal femoral joint region in one patient. A total of 96 previous surgical procedures had been performed in the 39 patients (Table I).
Table I.
Number of previous surgical procedures in patients (n = 39)
| Number of previous surgical procedures | Number of patients |
|---|---|
| 1 | 8 |
| 2 | 17 |
| 3 | 8 |
| 4 | 3 |
| 5 | 2 |
| 8 | 1 |
The healing process followed continuous curves; notably, there were no abrupt changes occurring when consolidation occurred. Interestingly, we also found that mechanically effective healing takes place several weeks before it is apparent radiographically.
Table II shows a statistical compilation of the detected measured values during the healing process. On average, 50% of the initial elasticity was measured after ten weeks, 25% of the initial elasticity was reached at 16 weeks and 10% of the initial elasticity was detected after 23 weeks. After 12 weeks, on average, an elasticity value of 38% of the inital value was measured. In all healed cases, an elasticity value of 10% or less of the initial elasticity was reached. Clinical union, defined as full weight-bearing in the absence of pain or tenderness,3 on average occurred shortly after the time point of 10% elasticity. The time point of 10% elasticity could retrospectively be correlated with clinical and radiological consolidation (correlation coefficient r = 0.83, p < 0.001).
Table II.
Statistics of the measured values during the bone healing process (n = 39)
| Time to 50% (wks) | Time to 25% (wks) | Time to 10% (wks) | Relative measurement value at 12 weeks (%) | Time to clinical consolidation (wks) | |
|---|---|---|---|---|---|
| Mean | 10.26 | 16.52 | 22.87 | 37.94 | 23.92 |
| Standard deviation | 5.68 | 9.83 | 12.84 | 26.35 | 7.70 |
| Median | 9.00 | 14.90 | 19.00 | 35.00 | 23.00 |
| Minimum | 3.50 | 4.00 | 4.50 | 0.00 | 12.71 |
| Quantil1 | 6.55 | 11.50 | 14.65 | 18.90 | 17.86 |
| Quantil3 | 12.25 | 18.75 | 27.50 | 53.00 | 28.86 |
| Maximum | 32.00 | 55.00 | 74.00 | 100.00 | 47.14 |
In total, four different types of healing curve could be distinguished. There were patients showing a fast decrease in elasticity resulting in bony healing within 12 weeks (Fig. 2). Others cases showed a slow decrease over several months, finally consolidating (Fig. 3). A different type of healing showed high elasticity values for a considerably long time, then suddenly showed consolidation (Fig. 4). A fourth type was related to the non-healing situation: the measured elasticity remained at a constantly high level (Fig. 5).
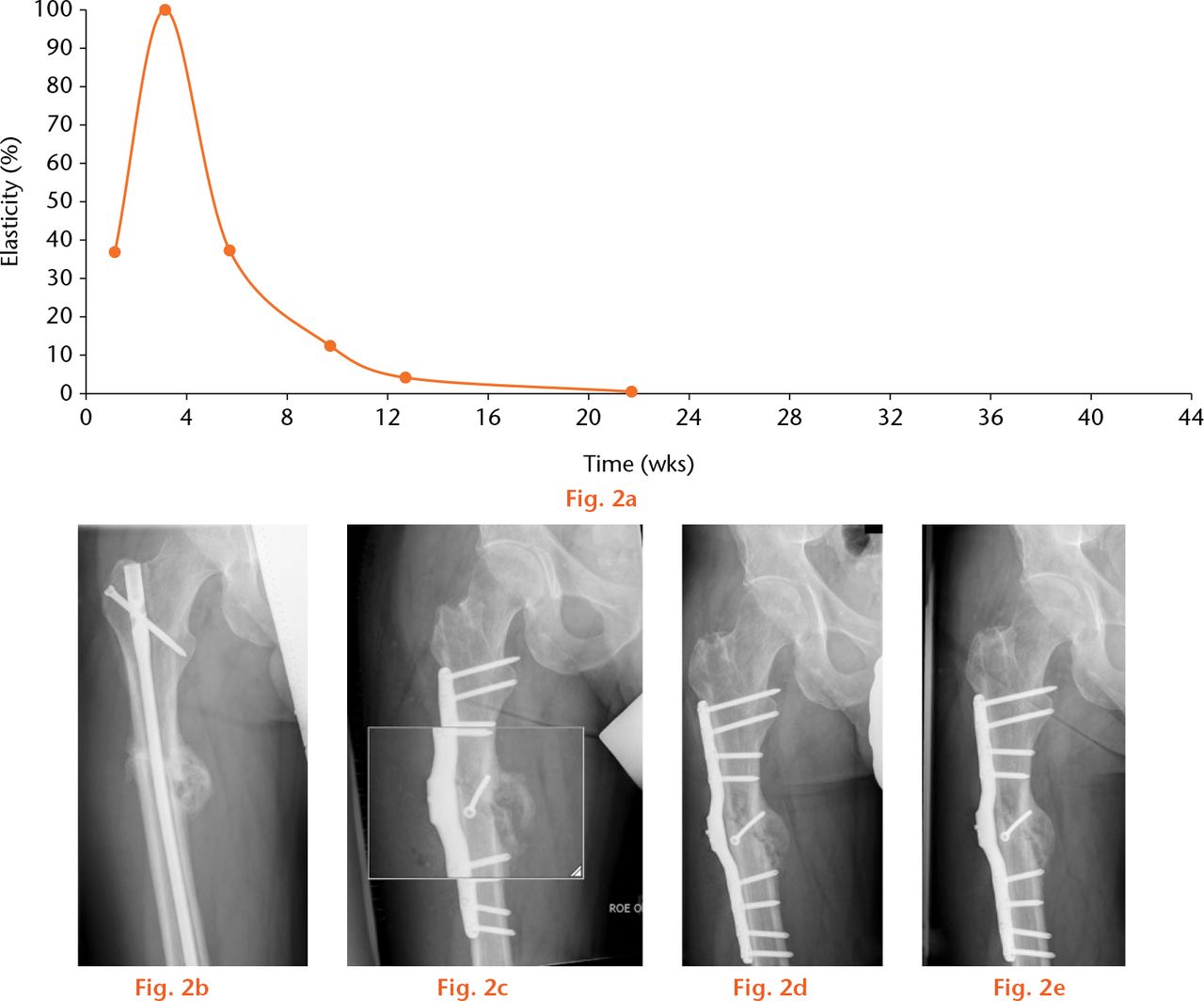
Fig.
Example of a fast healing nonunion. A 47-year-old patient was treated with the instrumented internal fixator for a delayed union, combined with a 17° internal torsional deformity six months after primary osteosynthesis with an unreamed nail and three months after dynamisation. In this graph, (a) the curve of the telemetrically measured elasticity of the osteosynthesis, anteroposterior radiographs (b) pre-operatively with a nail inserted, (c) immediately post-operatively, (d) five weeks post-operatively and (e) nine weeks post-operatively are shown. In this patient, a lag screw was applied, resulting in a high initial stability (low elasticity) which diminished at four weeks.
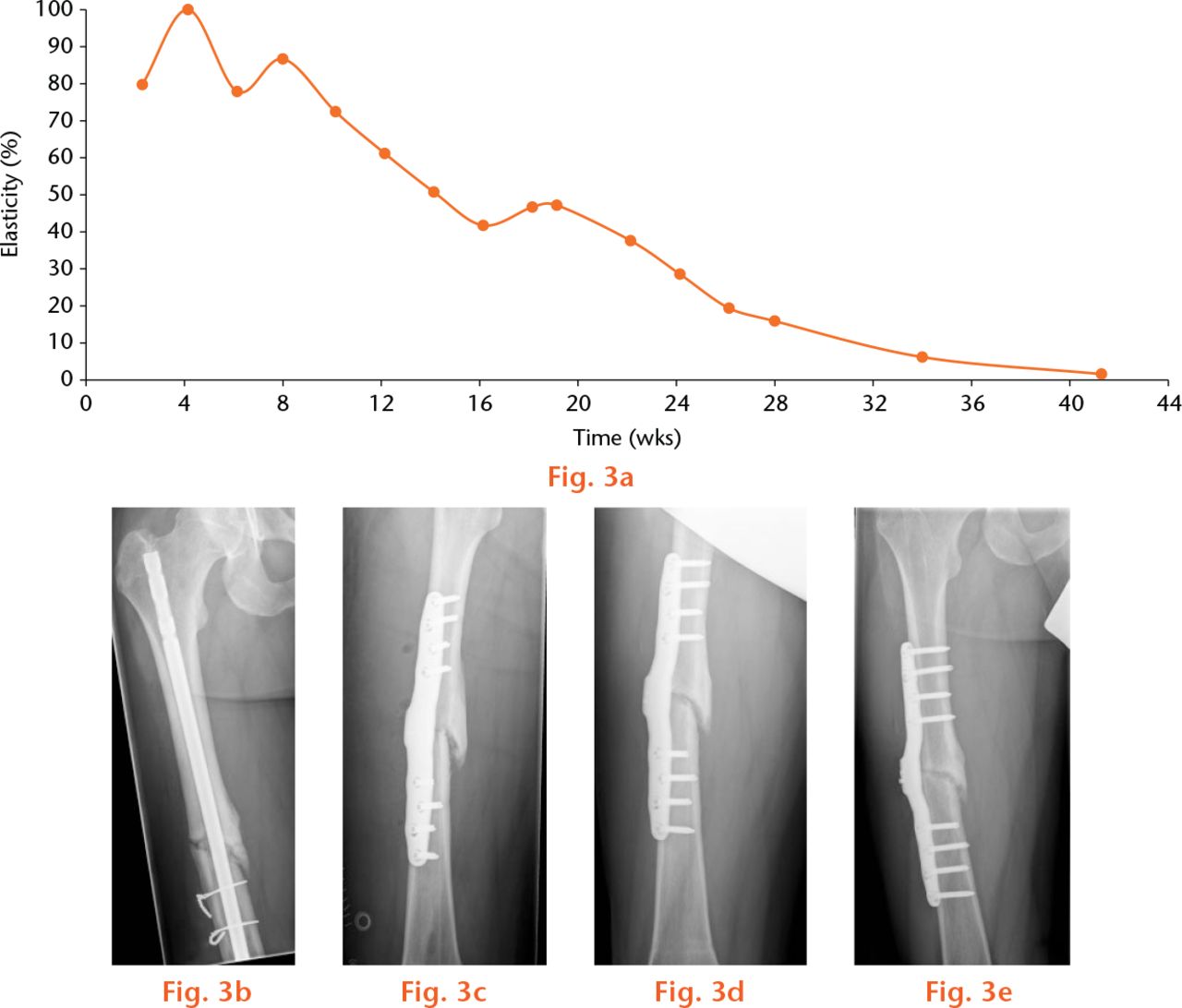
Fig.
Example of a slow healing nonunion. A 33-year-old patient was treated with the instrumented internal fixator for a nonunion 15 months after primary osteosynthesis with a T2 femoral nail and 12 months after dynamisation. In this graph, (a) the curve of the telemetrically measured elasticity of the osteosynthesis, anteroposterior radiographs (b) pre-operatively with a nail inserted, (c) immediately post-operatively, (d) 13 weeks post-operatively, (e) and 32 weeks post-operatively are shown.
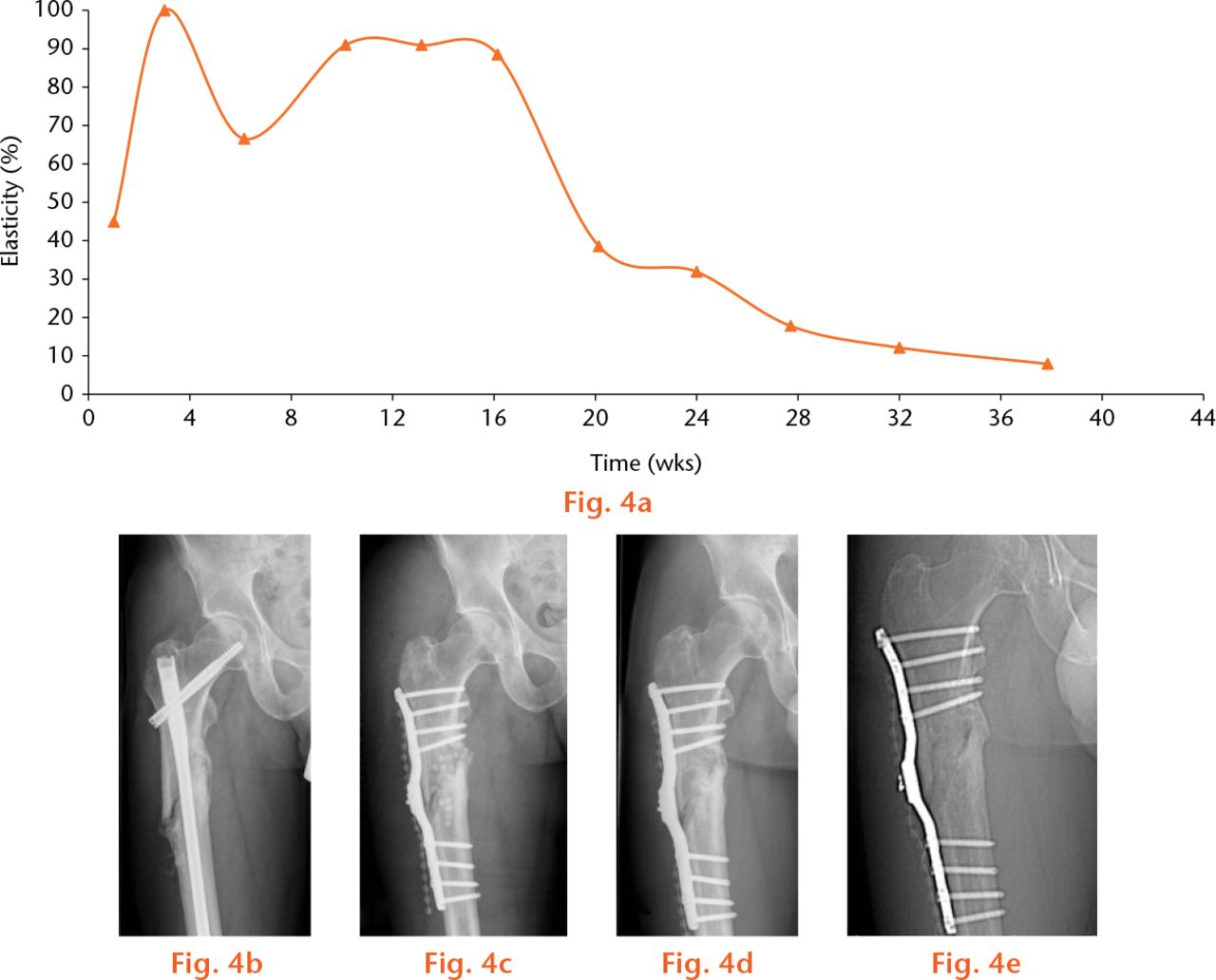
Fig.
Example of a ‘plateau’ healing nonunion. A 43-year-old patient was treated with the instrumented internal fixator for a nonunion 12 months after primary osteosynthesis with a gamma nail, followed by a revision four weeks later because of a 20° torsional deformity. In this graph, (a) the curve of the telemetrically measured elasticity of the osteosynthesis anteroposterior radiographs (b) pre-operatively with a nail inserted (c), immediately post-operatively, (d) 26 weeks post-operatively (e) and 32 weeks post-operatively are shown.
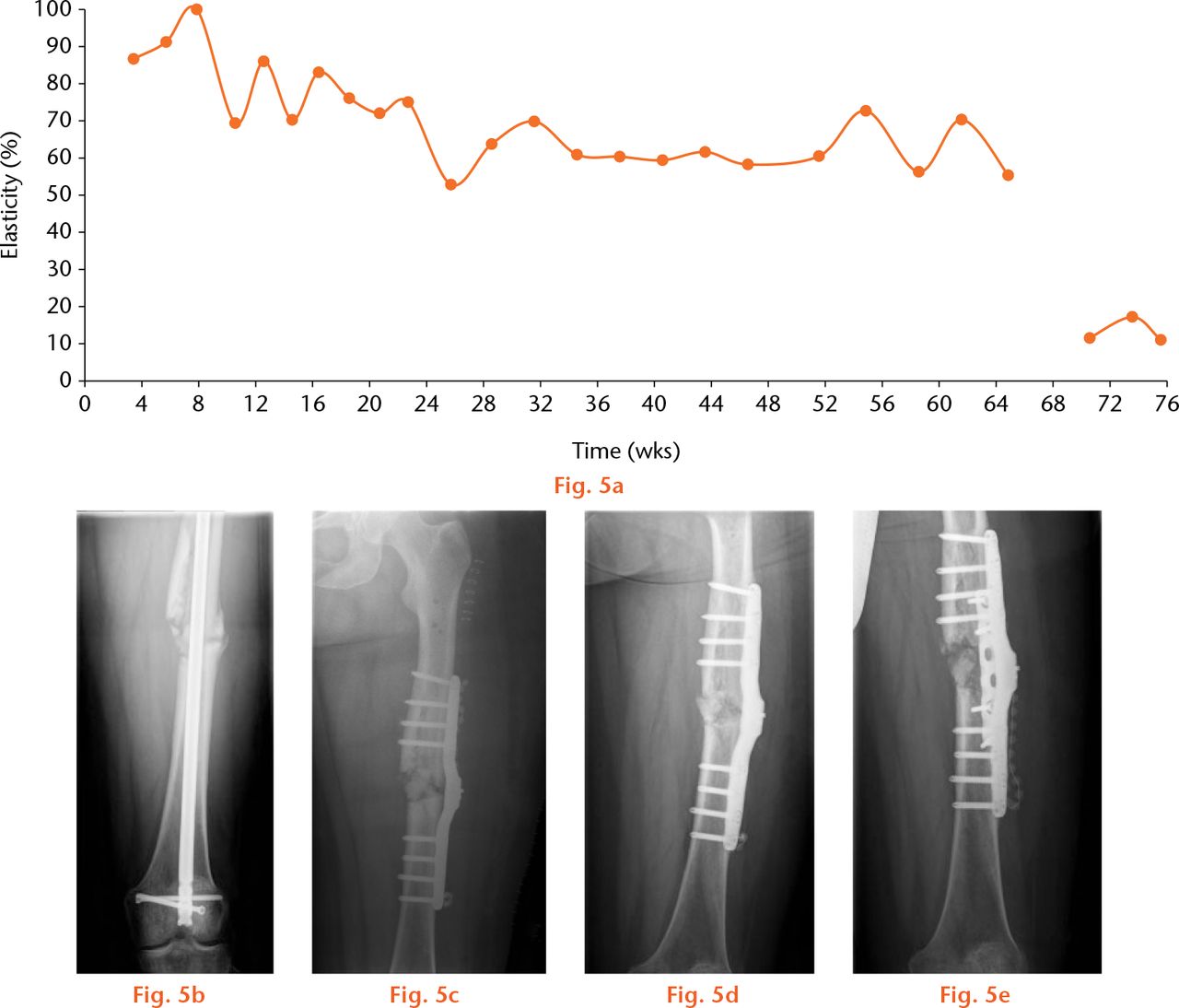
Fig.
Example of a non-healing nonunion. A 50-year-old patient was treated with the instrumented internal fixator for a nonunion eight months after a polytrauma with primary osteosynthesis with an unreamed nail and four months after dynamisation. In this graph, (a) the curve of the telemetrically measured elasticity of the osteosynthesis anteroposterior radiographs (b) pre-operatively with a nail inserted, (c) immediately post-operatively, and (d) 64 weeks post-operatively are shown. A revision was performed applying a cancellous bone graft and an additional plate (e) resulting in a significant decrease in elasticity.
A particularly important result of the clinical application was that re-operation could be avoided by means of the measurement curves. In the slow-healing patients, after six to eight months the question arose as to whether a revision surgery, such as a bone graft or re-stabilisation, would be indicated. In these patients, however, over the entire time course a continuously decreasing elasticity was observed, corresponding to a slowly increasing mechanical stabilisation. Therefore, the patients could be reassured and any intervention delayed. The further course of healing resulted in a definitive bony consolidation without the need for revision surgery.
Discussion
The electronically instrumented implant, also called “intelligent implant” because of the computer technology applied, has proven useful for the assessment of bone healing in complex clinical situations regarding the femur. In a previous publication,10 the correlation of the measured values with CT findings, the current benchmark, was shown. The measurements are therefore particularly suitable in order to reduce radiation exposure by performing successive CTs.
Telemetric measurements on orthopaedic implants have been previously described. Burny et al11 instrumented proximal thigh plates with strain gauges, first with transcutaneous wires, and later with telemetry electronics. Notably, it was shown that the rate of mechanical failures of the implants could be reduced, avoiding overload. Sommelet, Hummer and Ory12 introduced measurements with instrumented implants in 11 patients. However, the authors came to the conclusion that the measurements were extremely difficult to interpret and not clinically useful.
These historical findings contrast with our data indicating important clinical use. The discrepancy is likely due to the availability of modern locking implants. These implants provide a solid anchoring of the measurement system in the bone.13 In the earlier existing non-locking plate systems, the load transmission was not defined because of frictional effects and the movement of the screw heads in the plate. Therefore, we conclude that locking implants are necessary for the reliable measurement of implant strain forces.
This study did have an important limitation. Deviations of the measurements were observed due to the muscular tension of the patients. The three-times repeated execution of each measurement and inter-individual standardisation with respect to an initial value, rated as 100% minimised, but did not completely avoid, these deviations.
The electronically instrumented implant generates clinically valuable information. Patients with different courses of healing can be distinguished. The measurements can be especially helpful in the decision to avoid revision surgery. Another possible application is load monitoring during physiotherapy in order to avoid exercises with excessive loads which may be potentially harmful to the callus or the implant.9 Similarly, measuring the load in the implant can help direct progressive weight-bearing. However, larger studies would be needed to provide concrete directions in the progression of bearing weight. Automatic systems which evaluate the data and send an email to the patient’s mobile phone when detecting an overload are conceivable.14 The telemetrised implant is based on actual electronic parts from mass production. Therefore, cost-effective manufacturing and future routine application are indeed possible. Inevitably, the incorporation of microelectronics into orthopaedic implants will be an important future innovation in clinical care.
Supplementary material
Photographs showing the set-up of the telemetric system can be found alongside the paper at http://www.bjr.boneandjoint.org.uk/
Funding Statement
Funding has been received from DGUV and BMBF (German Mandatory Accident Insurance and German Federal Ministry of Education and Research) which is related to this article.
ICMJE conflict of interest
None declared.
References
1 Morshed S , CorralesL, GenantH, MiclauTIII. Outcome assessment in clinical trials of fracture-healing. J Bone Joint Surg [Am]2008;90(Suppl 1):62-67.CrossrefPubMed Google Scholar
2 Bhandari M , GuyattGH, SwiontkowskiMF, et al.. A lack of consensus in the assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma2002;16:562-566.CrossrefPubMed Google Scholar
3 Corrales LA , MorshedS, BhandariM, MiclauTIII. Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg [Am]2008;90-A:1862-1868.CrossrefPubMed Google Scholar
4 Brinker MR , O’ConnorDP. Nonunions: evaluation and Treatment. In: BrownerBD, LevineAM, JupiterJB, eds. Skeletal Trauma: basic science, management, and reconstruction. Philadelphia: Saunders Elsevier, 2009:615-708. Google Scholar
5 Davis BJ , RobertsPJ, MoorcroftCI, et al.. Reliability of radiographs in defining union in intramedullary fixation. Injury2004;35:557-561. Google Scholar
6 McClelland D , ThomasPB, BancroftG, MoorcraftCI. Fracture healing assessment comparing stiffness measurements using radiographs. Clin Orthop Relat Res2007;457:214-219.CrossrefPubMed Google Scholar
7 Nicholls PJ , BergE, BlivenFEJr, KlingJM. X-ray diagnosis of healing fractures in rabbits. Clin Orthop Relat Res1979;142:234-236.PubMed Google Scholar
8 Panjabi MM , LindseyRW, WalterSD, WhiteAAIII. The clinician’s ability to evaluate the strength of healing fractures from plain radiographs. J Orthop Trauma1989;3:29-32. Google Scholar
9 Faschingbauer M , SeideK, WeinrichN, et al.. Fixateur interne mit Telemetriesystem. Trauma Berufskrankh2007;9:88-97. (in German) Google Scholar
10 Seide K , AljudaibiM, WeinrichN, et al.. Telemetric assessment of bone healing with an instrumented internal fixator: a preliminary study. J Bone Joint Surg [Br]2012;94-B:398-404.CrossrefPubMed Google Scholar
11 Burny F , DonkerwolckeM, MoulartF, et al.. Concept, design and fabrication of smart orthopedic implants. Med Eng Phys2000;22:469-479.CrossrefPubMed Google Scholar
12 Sommelet J , HummerJ, OryJM. Méthode objective d’appréciation des déformations du complexe os-implant “in vivo” par télémesure. Acta Orthop Belg1976;42(Suppl):88-97. Google Scholar
13 Seide K , MorlockMM, SchümannU, WolterD. Wirkprinzipien der winkelstabilen Schrauben-Platten-Verbindung bei Fixateur-interne-Osteosynthesen. Trauma Berufsk1999;1:320-325.(Article in German.)[[bibmisc]] Google Scholar
14 Wolter D . Intelligentes Implantat“ Konzeption, gegenwärtige Realisation und zukünftiges Entwicklungspotential. Trauma Berufsk2007;9:74-76. (in German) Google Scholar









